What obesity management drugs mean for obtaining life insurance

New injectable medications used for weight reduction have recently been in the headlines. While a lot of the media coverage focuses on celebrities and reality stars using these medications to drop pesky pounds, the real news is that these medications are being used to treat chronic obesity in a new and successful way. As financial professionals, we see many of these medications are used on- and off-label. It’s essential that you understand the indications and learn about your client’s health journey before pursuing coverage.
Chronic obesity
Let’s start by discussing obesity. Many Americans are overweight (with a body mass index between 25 and 29.9) or obese (with a BMI of 30 or higher). The American Society for Metabolic and Bariatric Surgery further explains obesity as a chronic disease. “Obesity is no longer considered a cosmetic issue that is caused by overeating and a lack of self-control. The World Health Organization, along with national and international medical and scientific societies, now recognizes obesity as a chronic progressive disease resulting from multiple environmental and genetic factors. The disease of obesity is extremely costly not only in terms of economics but also in terms of individual and societal health, longevity, and psychological well-being. Due to its progressive nature, obesity requires life-long treatment and control.”
The shift of seeing obesity as a chronic disease and no longer a disease of character has changed the narrative about and approach to how the medical community and society view its treatment.
In the past, obese individuals were advised to eat less and move more. Other options, such as bariatric surgery and medications, were considered when diet and exercise didn’t work. Bariatric procedures such as gastric bypass, sleeve gastrectomy, duodenal switch and lap band have been used in the obese to surgically reduce overall excess weight by anywhere from 30% to 70%. These surgeries are invasive and life-changing (some can’t be undone), and many individuals are uncomfortable with this type of decision. These surgeries typically take months of preoperative workups and clearances and depend on the individual to make lifelong behavioral changes, which can prove challenging.
Over the years, multitudes of prescription medications and over-the-counter supplements have caused severe side effects such as heart valve damage, pulmonary hypertension, heart failure and even death. The obese population needed better treatment modalities.
Medication advancements
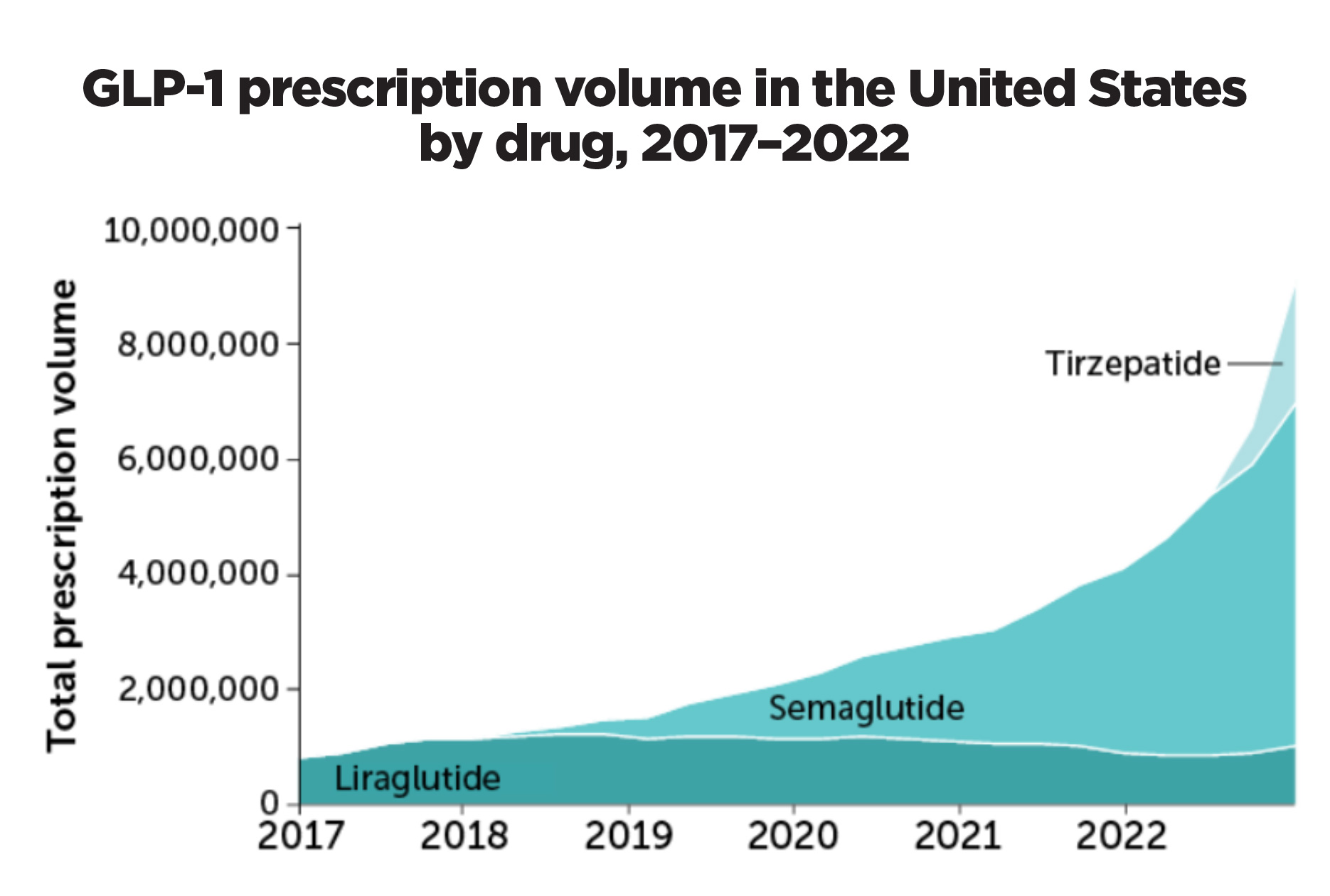
Medications such as Ozempic (semaglutide) and Mounjaro (tirzepatide) were being used for the treatment of Type 2 diabetes, but an interesting side effect — weight loss — was noted. For our discussion, we will stick to these two medications even though there are others. The U.S. Food and Drug Administration has approved variations of these medications for the treatment of obesity, and those branded names are:
• Wegovy, which is semaglutide, and the diabetic medication is Ozempic, a glucagon-like peptide-1 (GLP-1) agonist.
• Zepbound, which is tirzepatide, and the diabetic medication is Mounjaro, a gastric inhibitory polypeptide (GIP).
The mechanisms that made these medications effective for weight loss were called GIP and GLP-1 agonists; the various medications have one or a combination of these agonists named above. As Harvard Medical School explains the mechanism of GLP-1 agonists such as Wegovy, “GLP-1 is a hormone naturally released in the gastrointestinal tract in response to nutrient intake. It has multiple effects, including increasing insulin release from the pancreas, slowing down stomach emptying and targeting receptors in the brain that cause appetite reduction. This results in a sensation of satiety, or fullness, lasting much longer than possible with natural GLP-1 hormone levels.”
Zepbound works a little differently, as it combines GIP and GLP-1 agonists. The New England Journal of Medicine explained how Zepbound works. “Glucose-dependent insulinotropic polypeptide, another nutrient-stimulated hormone, regulates energy balance through cell-surface receptor signaling in the brain and adipose tissue. A molecule that combines both GIP and GLP receptor agonism theoretically may lead to greater efficacy in weight reduction.”
Various studies were completed before Wegovy and Zepbound were FDA-approved for treating obesity, showing that patients could expect to lose between 15% (with Wegovy) and 36.2% (with Zepbound) of excess weight. People taking these medications should eat healthily and increase their physical activity for optimal results.
Side effects
Ozempic has a long track record with people who have diabetes. Mounjaro is newer and has been FDA-approved for use by diabetics only since 2022. The FDA-approved versions of these medications (Wegovy and Zepbound) have a far shorter history.
Harvard Medical School notes the side effects of Wegovy. “The most common side effects of Wegovy are nausea, diarrhea, vomiting and constipation. The medication also comes with a warning for the risk of a specific tumor of the thyroid, and thus, it is not recommended for those with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia type 2 (a genetic condition associated with endocrine tumors). It should be noted that tumors were only observed in animal studies and not seen in the human trials.”
Eli Lilly and Company, the manufacturer of Zepbound, reported the associated side effects. “The most commonly reported adverse events (observed in less than 5% of clinical trial participants) were nausea, diarrhea, vomiting, constipation, abdominal pain, dyspepsia, injection-site reactions, fatigue, hypersensitivity reactions, eructation, hair loss, and gastroesophageal reflux disease… The label for Zepbound includes a boxed warning regarding thyroid C-cell tumors. Zepbound is contraindicated in patients with a personal or family history of medullary thyroid carcinoma, [and] in patients with multiple endocrine neoplasia syndrome type 2 ... .”
Although the most-mentioned side effects are gastrointestinal discomfort of different varieties, special attention should be paid to the other rare concerns that have been listed. As with any new medications, patients should do their homework before beginning use.
Controversy of shortages and barriers to use
The FDA approved Wegovy for obesity treatment on June 4, 2021, and the FDA approved Zepbound for obesity treatment on Nov. 8, 2023. Before those approvals, individuals seeking these medications were taking them off-label and tapping into the diabetic supply of Ozempic and Mounjaro. There have been shortages in the Ozempic and Mounjaro markets and the Wegvoy supply lines. These are expected to improve as production ramps up for the FDA-approved obesity medications.
Another controversy surrounding these medications is their usage in people who are not obese. The medications are considered therapeutic in the obese (BMI of 30 and up) or in the overweight (BMI between 27 and 29.9) with a weight-related condition such as diabetes, sleep apnea, cardiovascular disease, etc. The safety of these medications has not been studied in people with lower BMI ranges.
Cost is another factor for many. Some health insurers are slowly beginning to cover the cost of the medications for treating obesity, where it has been indicated, but not all insurers have agreed to do so.
The American Medical Association urges insurers to change their minds. “As a new generation of weight-loss medications has created additional options to treat obesity insurance coverage barriers limit the broad accessibility of these medications. In response, physicians and medical students voted to adopt a policy for the American Medical Association supporting health insurance coverage parity for evidence-based treatment of obesity, including FDA-approved medications without exclusions or additional carve-outs.”
The medications cost $1,000 a month or more without insurance, making the disparity of patients who have access to these medications quite vast.
Alcohol consumption
Some Wegovy users have found less urge to consume alcohol as well. This isn’t fully understood, but studies are underway to understand this better. As reported by NPR. “Studies in animals, as well as a few in people, offer tantalizing clues to how this mechanism works for both food and alcohol. Imagine for a second taking a bite of a chewy chocolate cookie. It’s buttery and very sweet.
“That first bite triggers the release of dopamine inside the part of your brain that controls your motivation,” says neuroscientist Alexandra G. DiFeliceantonio, an assistant professor at Virginia Tech. “But studies have found that in animals and people, GLP-1 drugs reduce the release of dopamine in this region when you eat something sweet and fatty or when you consume alcohol.” The medical world anxiously awaits the outcome of the research in this vein.
Cardiovascular disease
Another potential benefit of semaglutide has been published recently. Cleveland Clinic stated, “Findings from a multi-center, international clinical trial reported by a Cleveland Clinic physician show that semaglutide reduced cardiovascular events by 20% in adults with overweight or obesity and established cardiovascular disease who don’t have diabetes.” This study illuminates another positive impact of using semaglutide and is promising for the medical field.
Chronic disease management
A central argument for the continued use of these new medications is that people regain most of the weight lost after they discontinue the medication. The medication should be prescribed with the understanding that this is a medication for chronic disease. Just as it isn’t recommended to stop taking hypertensive or thyroid medications once control is attained, these medications shouldn’t be discontinued once the desired weight loss is achieved. These medications should be viewed as maintenance medications.
Field underwriting is always critical to meeting client expectations. When gathering information on clients’ medical history, please be sure to ask:
• Current height and weight.
• Has there been any weight loss in the past 12 months? If so, how much? How did they lose this weight (e.g., diet, exercise, medications)?
• When asking what medications a client takes, please determine the medical diagnosis for the medication(s) being taken, as there can be multiple indications on- and off-label.
The underwriting decision will be determined after reviewing the weight lost within the past 12 months in addition to any other underwriting information developed upon review.
Emily Bancroft, MS, Certified FALU, FLMI, AIRC, ACS, is senior underwriter, Crump Insurance Services. Contact her at [email protected].






Removing roadblocks to choosing annuities
Thrive and grow: 4 ways to protect and grow your business
Advisor News
- The best way to use a tax refund? Create a holistic plan
- CFP Board appoints K. Dane Snowden as CEO
- TIAA unveils ‘policy roadmap’ to boost retirement readiness
- 2026 may bring higher volatility, slower GDP growth, experts say
- Why affluent clients underuse advisor services and how to close the gap
More Advisor NewsAnnuity News
- Pinnacle Financial Services Launches New Agent Website, Elevating the Digital Experience for Independent Agents Nationwide
- Insurer Offers First Fixed Indexed Annuity with Bitcoin
- Assured Guaranty Enters Annuity Reinsurance Market
- Ameritas: FINRA settlement precludes new lawsuit over annuity sales
- Guaranty Income Life Marks 100th Anniversary
More Annuity NewsHealth/Employee Benefits News
- The Health Care Cost Curve Is Bending up Again
- Republicans can make healthcare affordable by focusing on insurance reforms
- Governor Stitt strengthens regulations for Medicare Advantage Plans
- Health insurance CEO can't commit to safe AI practices in Congressional hearing
- Harshbarger presses insurance CEOs on market control, vertical integration, conflict of interest
More Health/Employee Benefits NewsLife Insurance News