Medicaid unwinding: How is it impacting the health care markets?
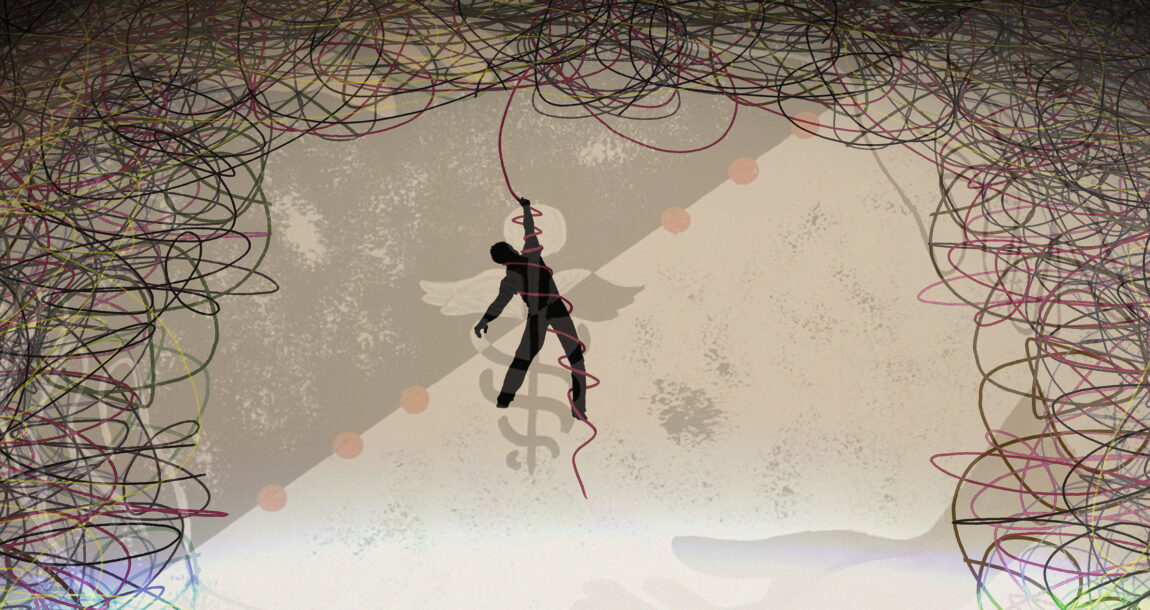
The Medicaid unwinding began one year ago this week, and the impact of millions of Americans being disenrolled from Medicaid coverage will continue to be felt into the next few years.
The American Academy of Actuaries looked into the Medicaid unwinding’s impact on the health care markets in 2024 during a recent webinar.
During the pandemic, states were prohibited from disenrolling people from Medicaid in exchange for an increase in federal Medicaid matching payments, explained Jennifer Tolbert with KFF’s Program on Medicaid and the Uninsured. Congress passed the Consolidated Appropriations Act in December 2022, ending the continuous enrollment provision on March 31, 2023, and phasing down enhanced federal matching payments through Dec. 31, 2023.
States could resume disenrolling people from Medicaid starting April 1, 2023, but first had to conduct a full renewal in accordance with federal rules before terminating coverage.
Medicaid enrollment reached a high of 94 million in April 2023, but declined each month since then, finishing 2023 with 85 million enrollees. More than 19 million have been disenrolled from Medicaid as of late March. In addition, 46 million people had their Medicaid coverage renewed while another 34.3 million renewals are yet to be determined.
The states still have a way to go in completing the unwinding, Tolbert said. Some states delayed the start of their unwinding until June or July 2023, while some paused or slowed the pace of disenrollment during the unwinding period.
70% disenrolled due to procedural reasons
Of those who were disenrolled from Medicaid, 70% were disenrolled for procedural reasons, Tolbert said. Procedural disenrollment can happen for a variety of reasons, she said.
“Maybe someone didn’t receive their renewal notice or they weren’t able to gather the required documentation and return it within the required timeframe,” she said. “Some may have started a new job and enrolled in employer coverage, so they may have chosen not to complete the renewal process.”
But many who were disenrolled for procedural reasons may still be eligible for Medicaid coverage, she added, and might not realize they were dropped from coverage until they try to access care.
As of December 2023, about 28% of those disenrolled from Medicaid transitioned to coverage on the Affordable Care Act marketplace, Tolbert said. But many people disenrolled from Medicaid will become uninsured, even if they re-enroll in Medicaid or obtain other coverage, KFF research showed.
As the unwinding continues, a number of key questions remain, Tolbert said.
- What are the characteristics of people who have been disenrolled from Medicaid? How do their health status and health needs compare with those who have maintained Medicaid coverage?
- What strategies have been most effective at reducing procedural disenrollments and churn (moving back onto Medicaid after being disenrolled)?
- How will unwinding affect overall Medicaid enrollment and health coverage rates, particularly the uninsured rate?
Actuarial considerations of the unwinding
The Medicaid unwinding has several considerations for actuaries, said Colby Schaeffer of the American Academy of Actuaries’ Medicaid Committee. Among those considerations:
- Large changes in total enrollment between the pre-public health emergency, the PHE and the post-unwinding periods will result in a changing mix of Medicaid enrollees with varying usage patterns.
- The average risk profile of Medicaid enrollees is notably different between the PHE and post-unwinding periods. Those who may already have other health insurance coverage dilute the risk profile during the PHE. Eligibility redeterminations that lead to the disenrollment of non-utilizers will remove the dilution, resulting in an increase to expected per capita costs.
- The average risk profile can be thought of us acuity, which is the average cost of a cohort of individuals due to their underlying risk that drives usage of health care services.
Susan Rupe is managing editor for InsuranceNewsNet. She formerly served as communications director for an insurance agents' association and was an award-winning newspaper reporter and editor. Contact her at Susan.Rupe@innfeedback.com. Follow her on X @INNsusan.
© Entire contents copyright 2024 by InsuranceNewsNet.com Inc. All rights reserved. No part of this article may be reprinted without the expressed written consent from InsuranceNewsNet.com.





Consumer groups address ‘shortcomings’ in CMS prior authorization ruling
Insuring the future: Why agility is key in a changing climate
Advisor News
- Study asks if annuities help financial advisors build client relationships
- California’s big pension funds lost billions in stock market selloff. Can they recover in time?
- Economist: Tariffs could dampen GDP growth; raise unemployment, inflation
- Medium tenure for workers remains at about 5 years
- Making the most of Financial Literacy Month
More Advisor NewsAnnuity News
- Emerging digital annuity sales process cutting cycle times by 94%, IRI says
- In times of market volatility, FIAs make the difference
- Charitable gift annuities gaining in popularity
- Nationwide and Annexus establish first actively managed mutual fund within a RILA
- AM Best Comments on the Credit Ratings of Talcott Financial Group Ltd.’s Subsidiaries Following Announced Reinsurance Transaction With Japan Post Insurance Co., Ltd.
More Annuity NewsHealth/Employee Benefits News
- Rural Hospitals Question Whether They Can Afford Medicare Advantage Contracts
- Brandeis University Reports Findings in Drugs Used In Alcohol Dependence (Alcohol Use Disorder Medication Coverage and Utilization Management In Medicaid Managed Care Plans): Drugs and Therapies – Drugs Used In Alcohol Dependence
- Minnesota couple accused of cheating Medicaid and Medicare of millions, buying mansion
- Health Insurance Shares Climb After Medicare Reimbursements are Boosted
- Medicaid expansion at risk: 'My life was saved by the citizens of Ohio'
More Health/Employee Benefits NewsLife Insurance News
- Proxy Statement (Form DEF 14A)
- Jackson Announces New President and Chief Risk Officer
- Proxy Statement (Form DEF 14A)
- Proxy Statement (Form DEF 14A)
- AM Best Revises Issuer Credit Rating Outlook to Stable for Life Insurance Company of Alabama
More Life Insurance News