COVID-19 Made A Mental Health Crisis Even Worse, EBRI Speakers Say
The COVID-19 pandemic “is a defining moment in a series of defining issues” regarding the mental health of American workers and their families.
That was the word from Katy Riddick, senior director of One Mind At Work, who spoke at the Employee Benefit Research Institute Spring Policy Forum.
Workers were struggling with mental health before the pandemic hit, she said, and found a lack of mental health support during that time. COVID-19 introduced new pressure to workers or exacerbated existing issues. Making things worse, she said, is that many people have experienced trauma, grief and loss as a result of the pandemic and resulting shutdown.
“We were in the midst of a mental health crisis before the pandemic,” Riddick said. “But we added to that a whole set of new challenges and asked people to adjust in broad societal measures as well as in individual circumstances.”
Twenty percent of employees report they are experiencing symptoms of depression, she said, while 5% say they are living with depression.
The pandemic also brought a change in the way employers view mental health, Riddick said. Previously, employers responded to workers who suffered with an acute mental health issue or serious mental illness. Now employers are showing a greater focus on the entire workforce.
“Every person in your organization brings mental health to work every day; they all could benefit from help,” she said.
Employers are responding to their workers’ mental health in a three-pronged approach, Riddick said.
- Be aware. Address cultural and workflow expectations along with health benefits.
- Be informed. Strategize mental health support around emerging expectations regarding the employer’s role, and measure the impact of programs.
- Be an example. Lead by example by modeling self-care behaviors and creating a supportive environment.
Diagnosis Rates, Spending Going Up
The percentage of the population under age 65 who are diagnosed with mental health disorders increased between 2013 and 2020, but it’s possible those rates are underreported. Paul Fronstin, EBRI’s director of health research, said the percentage of those under 65 diagnosed with mental health disorders increased to 18.5% in 2020 from 14.2% in 2013, according to health insurance claims data.
But Fronstin said he believes those rates are underreported for two reasons: 1) stigma surrounding discussion of mental health, and 2) the diagnosis code for the person seeking treatment was not always associated with a mental health issue.
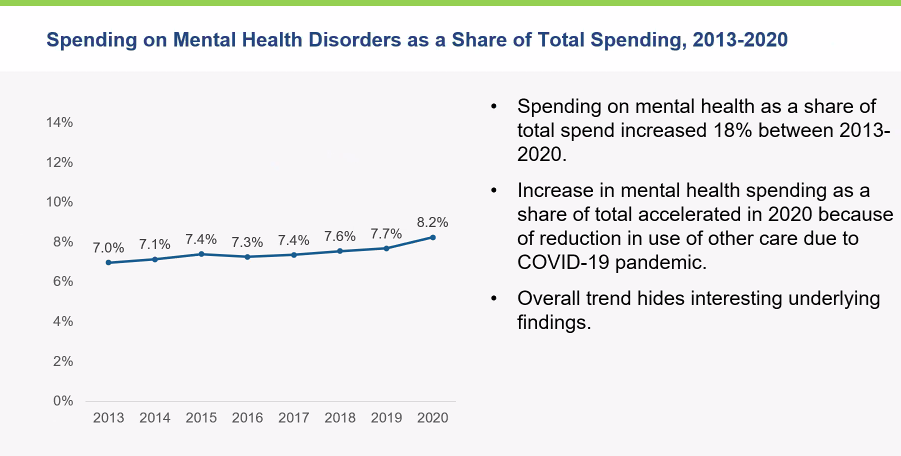
Spending on mental health has been ticking upward between 2013 and 2020, EBRI research revealed. Spending on mental health disorders as a share of total health care spending increased from 7% in 2013 to 8.2% in 2020. Inpatient and outpatient mental health care saw increases in spending during that time, Fronstin said, while spending on prescription drugs for mental health fell.
Workers Seeking Help
One in four Americans enrolled in employer-provided coverage – 41 million individuals – received mental health support in 2020, according to research from America’s Health Insurance Plans. That figure includes 6 million children, said Adam Beck, AHIP’s vice president, employer health policy & initiatives.
Telehealth appointments for mental health treatment increased 100-fold in 2020, he added.
AHIP’s findings were based on employer-provided insurance claims for workers and their covered dependents.
Of those who received mental health treatment in 2020, 13 million enrollees received individual and group psychotherapy, 22 million received treatment by primary care physicians, and 31 million obtained prescription drugs.
What will the future bring to mental health and employer-provided coverage? Beck provided a list of AHIP’s goals:
- Grow the number of licensed mental health professionals nationwide.
- Increase participation of mental health providers in health insurance networks.
- Expand the use of telehealth services.
- Address social determinants of health.
- Better integrate mental health into primary care visits and evaluations.
Susan Rupe is managing editor for InsuranceNewsNet. She formerly served as communications director for an insurance agents' association and was an award-winning newspaper reporter and editor. Contact her at [email protected]. Follow her on Twitter @INNsusan.
© Entire contents copyright 2022 by InsuranceNewsNet.com Inc. All rights reserved. No part of this article may be reprinted without the expressed written consent from InsuranceNewsNet.com.
Susan Rupe is editor in chief, magazine, for InsuranceNewsNet. She formerly served as communications director for an insurance agents' association and was an award-winning newspaper reporter and editor. Contact her at [email protected].






Guardian Life Develops New Dental Insurance Offerings
What ‘COVID Clarity’ Has To Do With The Great Resignation
Advisor News
- NAIFA: Financial professionals are essential to the success of Trump Accounts
- Changes, personalization impacting retirement plans for 2026
- Study asks: How do different generations approach retirement?
- LTC: A critical component of retirement planning
- Middle-class households face worsening cost pressures
More Advisor NewsAnnuity News
- Edward Wilson Joins SEDA, Bringing Deep Expertise in Risk Management, Derivatives Trading and Institutional Prime Brokerage
- Trademark Application for “INSPIRING YOUR FINANCIAL FUTURE” Filed by Great-West Life & Annuity Insurance Company: Great-West Life & Annuity Insurance Company
- Jackson Financial ramps up reinsurance strategy to grow annuity sales
- Insurer to cut dozens of jobs after making splashy CT relocation
- AM Best Comments on Credit Ratings of Teachers Insurance and Annuity Association of America Following Agreement to Acquire Schroders, plc.
More Annuity NewsLife Insurance News
Property and Casualty News
- Expedited final ruling holding up $4B settlement distribution
- GOVERNOR HOCHUL UNVEILS GRASSROOTS SUPPORT BEHIND HER PROPOSALS TO LOWER THE COST OF AUTO INSURANCE
- SNEED ADVANCES FOUR INSURANCE BILLS IN COMMITTEE
- Bills to rein in home insurance costs fail to advance in Oklahoma Legislature
- Louisiana’s fortified roof grant program can’t keep up with demand from homeowners
More Property and Casualty News