Most long-term care doesn’t qualify for insurance benefit

The U.S. Department of Health and Human Services’ latest report on long-term care projected a lower likelihood of requiring LTC and highlighted a new issue for financial professionals: The majority of LTC may be needed by clients who have lower levels of disability that do not meet the criteria for an LTC insurance benefit. The report’s authors concluded that better financial planning is needed to deal with the costs of LTC across the entire spectrum of disability at older ages.
LTC estimates were based on a microsimulation model that estimated the likelihood and duration of LTC for individuals (not couples, as explained further) who turned 65 today. The benchmark in the study, as with prior government studies that modeled LTC risk, was significant disability that required care at “the threshold for benefits under a tax-qualified long-term care insurance policy as specified by the Health Insurance Portability and Accountability Act (HIPAA)” of 1996. This advanced level of disability is what financial professionals target when they discuss LTC with clients. LTC at earlier levels of disability is not usually included in planning strategies.
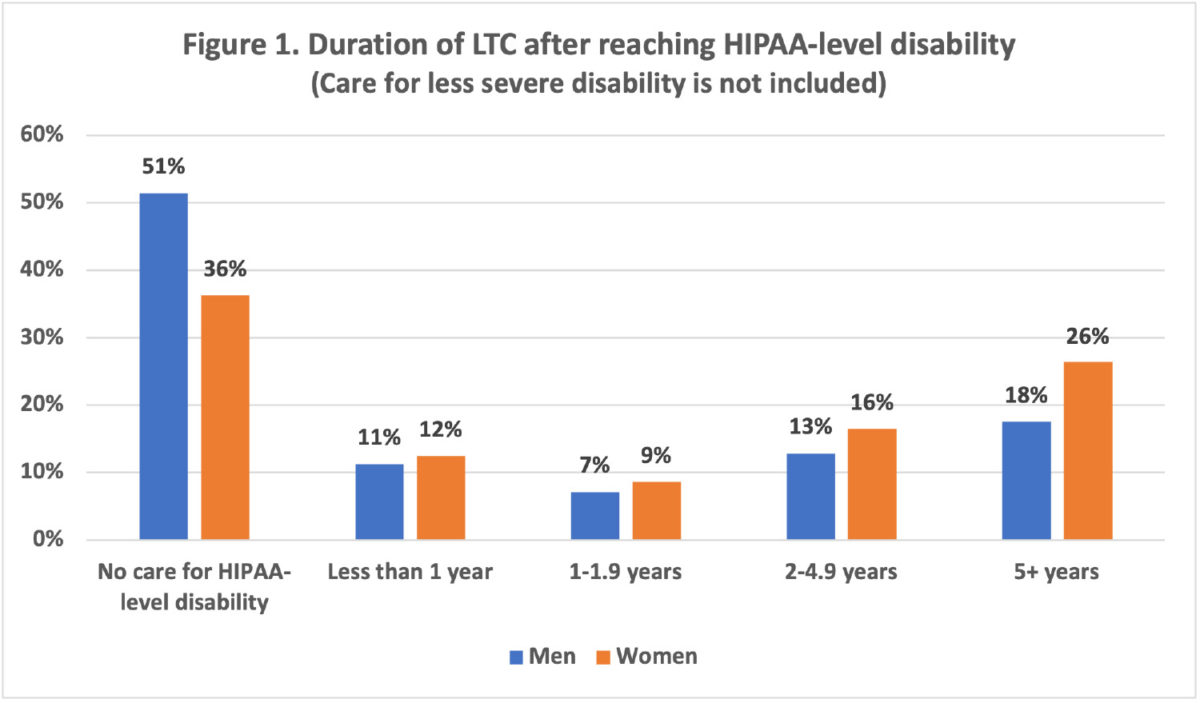
Estimates for significant disability at the HIPAA threshold were as follows.
» Forty-nine percent of men and 64% of women turning 65 today will require long-term care.
» For all 65-year-olds combined, including those who will and will not need LTC, the duration of LTC will average 3.1 years.
» If projections included only people who will need LTC, the duration of LTC will average 5.4 years.
Figure 1 shows the distribution of LTC by duration.
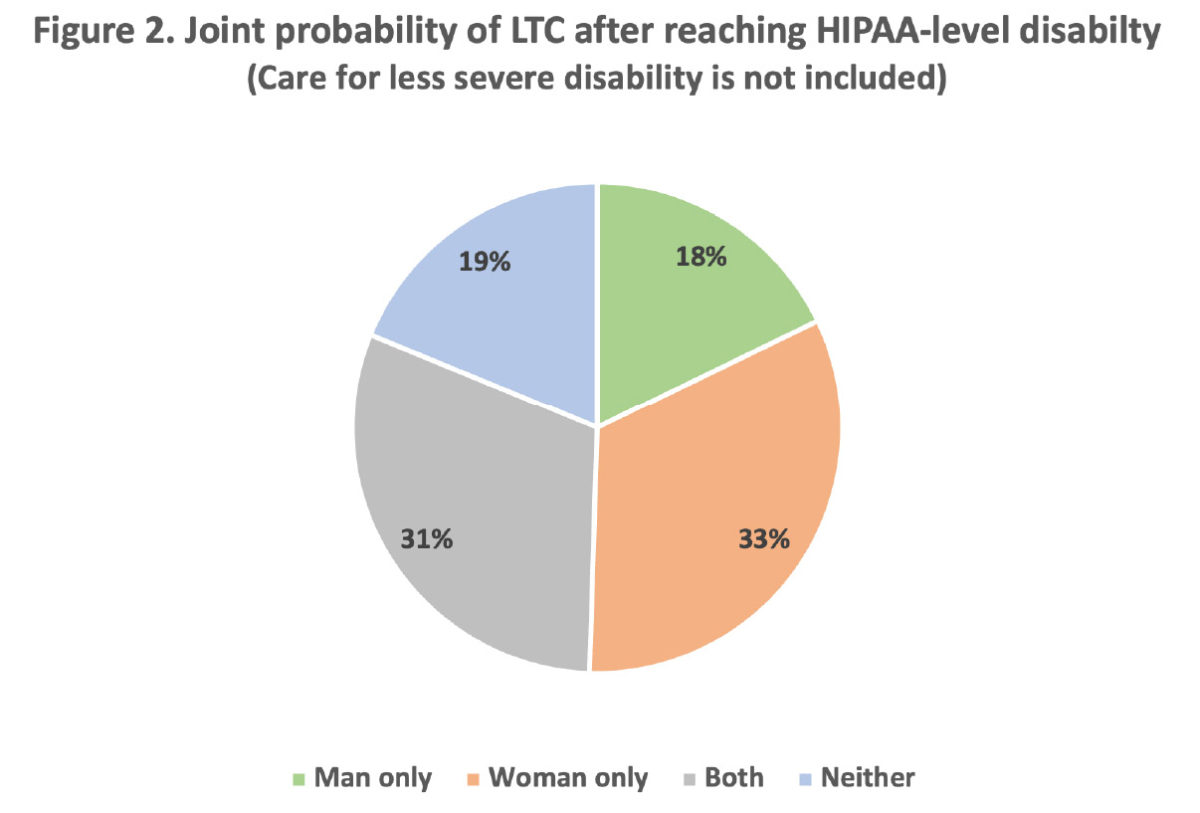
Data from the study was used to calculate the joint probability of LTC in couples (Figure 2). In eight out of 10 couples (81%), one or both partners will need LTC after reaching HIPAA-level disability.
The report highlighted a second issue of importance to financial professionals: Projections in the study underestimated the true likelihood and cost of LTC. The reason is because this and most similar studies do not count LTC that is provided before reaching HIPAA-level disability, which includes:
» LTC due to limitations of the instrumental activities of daily living (cooking, housework, laundry, managing finances and medical care, phone and computer use, shopping, and transportation).
» LTC because of inability to do one activity of daily living, rather than the two or more ADL limitations required by HIPAA criteria.
» LTC for some significant disabilities that can be mitigated with special equipment, such as wheelchairs, walkers, handrails and ramps.
How common is pre-HIPAA-level LTC? An earlier study by the Urban Institute suggested that the majority of LTC may be provided for people with lower levels of disability who do not meet the threshold for an LTC insurance benefit. Estimates are that one in four people (26%) who pay for LTCi and almost three in four (71%) who receive only unpaid LTC would not meet the threshold for benefits under a tax-qualified LTC insurance policy.
Health care and social service professionals have largely abandoned the expression “long-term care” because this term is associated with end-of-life care for severe disability. The preferred designation today is “long-term services and supports,” which includes a much broader array of unpaid and paid services that are needed as a result of aging, chronic illness or disability.
Points of engagement
» Financial professionals generally equate LTC with advanced disability that satisfies the benefit criteria of a tax-qualified LTCi policy. This approach creates an artificial distinction between LTC that is provided before and after meeting HIPAA criteria.
» For clients, LTC is not a “Yes or No” dichotomy that is determined by an arcane government law or an insurer’s benefit criteria. Instead, LTC is experienced as a continuum of care that evolves as disability worsens over time. It begins when care is first needed and costs are incurred.
» The majority of LTC may be needed at lower levels of disability that can exhaust family caregivers and deplete retirement funds. Some clients will never reach a point where their illness triggers an LTCi benefit, usually because death occurs at an earlier stage of disability.
» Recognition of the need for LTC at earlier stages of disability presents novel planning opportunities for financial professionals. The messages are that (1) LTC will be needed by the majority of individuals, and the likelihood is even higher for couples, (2) care will usually involve both unpaid (family) and paid caregivers, and (3) much, and sometimes all, of the care and cost will be incurred at lower levels of disability. This message ideally should be included in the financial plan, especially for single clients, widows, and couples with limited financial means who could spend down their assets before reaching the threshold for an LTCi benefit.
This more holistic approach to LTC planning will reassure clients that financial professionals are concerned about the impact of LTC across the entire spectrum of disability. Some clients will still have no interest in LTC planning. But merely introducing this topic often will lead to discussions about investments, wealth transfer, financial planning, closer ties to adult children who will be the main caregivers and potential clients in the future, as well as product options, including life and LTC insurance, annuities and Medicare supplement insurance.



This overlooked asset could help optimize your clients’ financial plan
A life lesson in success — with John Wheeler
Advisor News
- TIAA, MIT Age Lab ask if investors are happy with financial advice
- Youth sports cause parents financial strain
- Americans fear running out of money more than death
- Caregiving affects ‘sandwich generation’s’ retirement plans
- Why financial consciousness is the key to long-term clarity
More Advisor NewsAnnuity News
Health/Employee Benefits News
- Expiring health insurance tax credits loom large in Pennsylvania
- Confusion muddies the debate over possible Medicaid cuts
- Trump protesters in Longview aim to protect Medicaid, democracy, due process
- Grant Cardone, Gary Brecka, settle dueling state lawsuits
- 9 in 10 put off health screenings and checkups
More Health/Employee Benefits NewsLife Insurance News
- ‘Really huge’ opportunity for life insurance sales if riddle can be solved
- Americans fear running out of money more than death
- NAIFA eyes tax reform, retirement issues in 2025
- Legislation would change tax treatment of life insurers’ debt investments
- Closing the life insurance coverage gap by investing in education
More Life Insurance News