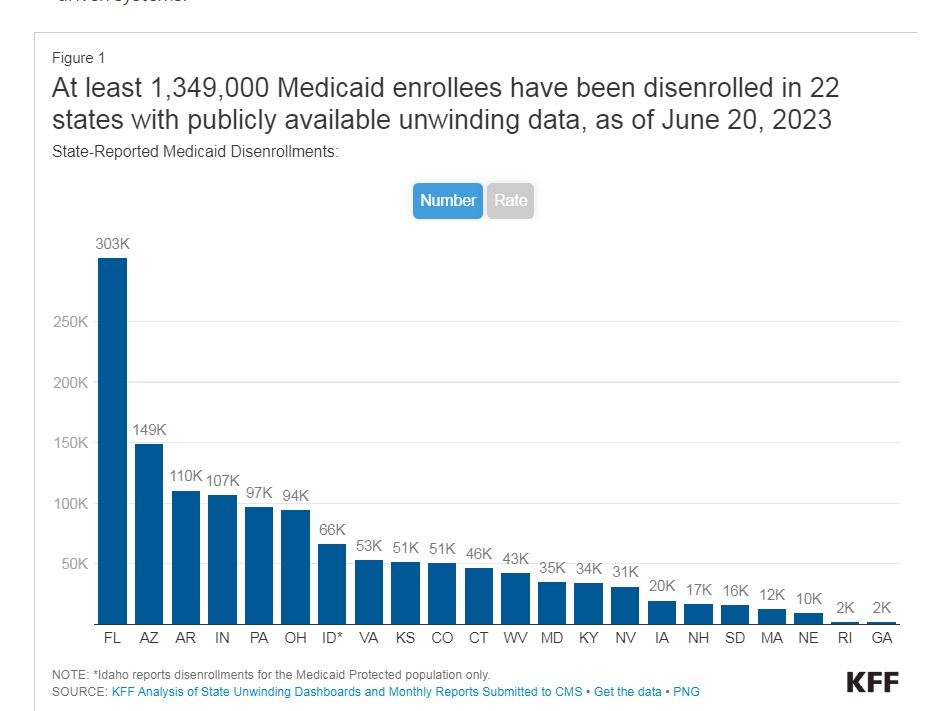
Medicaid unwinding: At least 1.3M enrollees lose coverage

At least 1.34 million Medicaid enrollees have been disenrolled as of June 20, based on the most current data from 22 states, KFF reports. The unwinding data are pulled from state websites, where available, and from the Centers for Medicare & Medicaid Services.
Overall, 35% of people with a completed renewal were disenrolled in reporting states while 65%, or 2.5 million enrollees, had their coverage renewed (three of the 22 reporting states do not provide data on renewed enrollees). Because not all states have publicly available data on total disenrollments, the data reported here undercount the actual number of disenrollments.
To view data for specific states, click on the State Enrollment and Unwinding Data tab.
There is wide variation in disenrollment rates across reporting states, ranging from 73% in Idaho to 16% in Virginia.
For Idaho, the disenrollment rate is among only those enrollees whose coverage was maintained during the pandemic and who the state believes are no longer eligible, which may explain, in part, the higher disenrollment rate.
Differences in who states are targeting with early renewals as well as differences in renewal policies and systems capacity likely explain some of the variation in disenrollment rates. Some states are initially targeting people early in the unwinding period that they think are no longer eligible or who did not respond to renewal requests during the pandemic, but other states are conducting renewals based on an individual’s renewal date.
Additionally, some states have adopted several policies that promote continued coverage among those who remain eligible and have automated eligibility systems that can more easily and accurately process renewals while other states have adopted fewer of these policies and have more manually-driven systems.
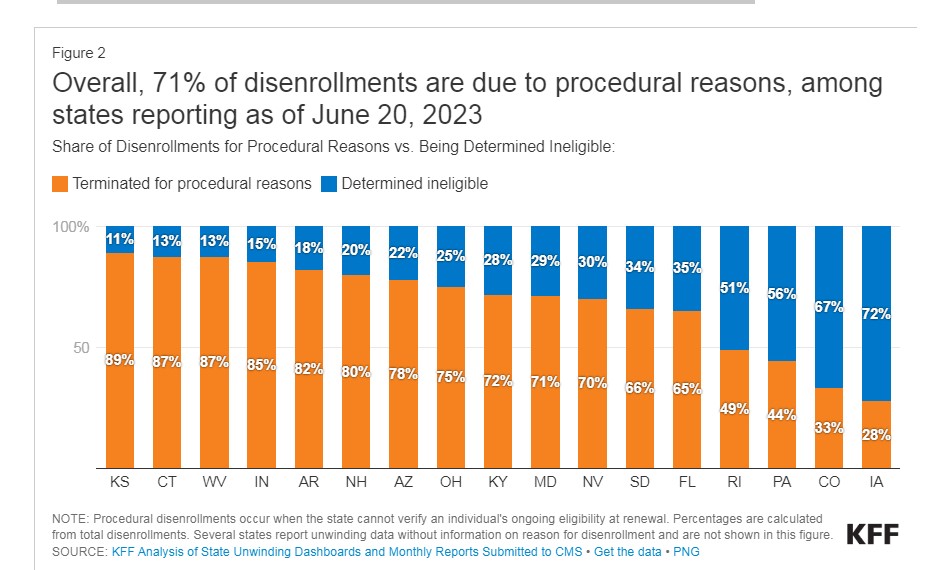
Across all states with available data, 71% of all people disenrolled had their coverage terminated for procedural reasons. There is also wide variation in rates of procedural disenrollments across states reporting this breakout, ranging from 89% in Kansas to 28% in Iowa.
Procedural disenrollments are cases where people are disenrolled because they did not complete the renewal process and can occur when the state has outdated contact information or because the enrollee does not understand or otherwise does not complete renewal packets within a specific timeframe. High procedural disenrollment rates are concerning because many people who are disenrolled for these paperwork reasons may still be eligible for Medicaid coverage.
Background on the unwinding of the Medicaid continuous enrollment provision
The Medicaid continuous enrollment provision, which had halted Medicaid disenrollments since March 2020, ended on March 31, 2023. Primarily due to the continuous enrollment provision, KFF estimates that enrollment in Medicaid/CHIP grew by 23.3 million to nearly 95 million from February 2020 to the end of March 2023. As states unwind the continuous enrollment provision over the following 12 months, they will redetermine eligibility for all Medicaid enrollees and will disenroll those who are no longer eligible or who may remain eligible but are unable to complete the renewal process. Millions of people are expected to lose Medicaid coverage during this unwinding period.
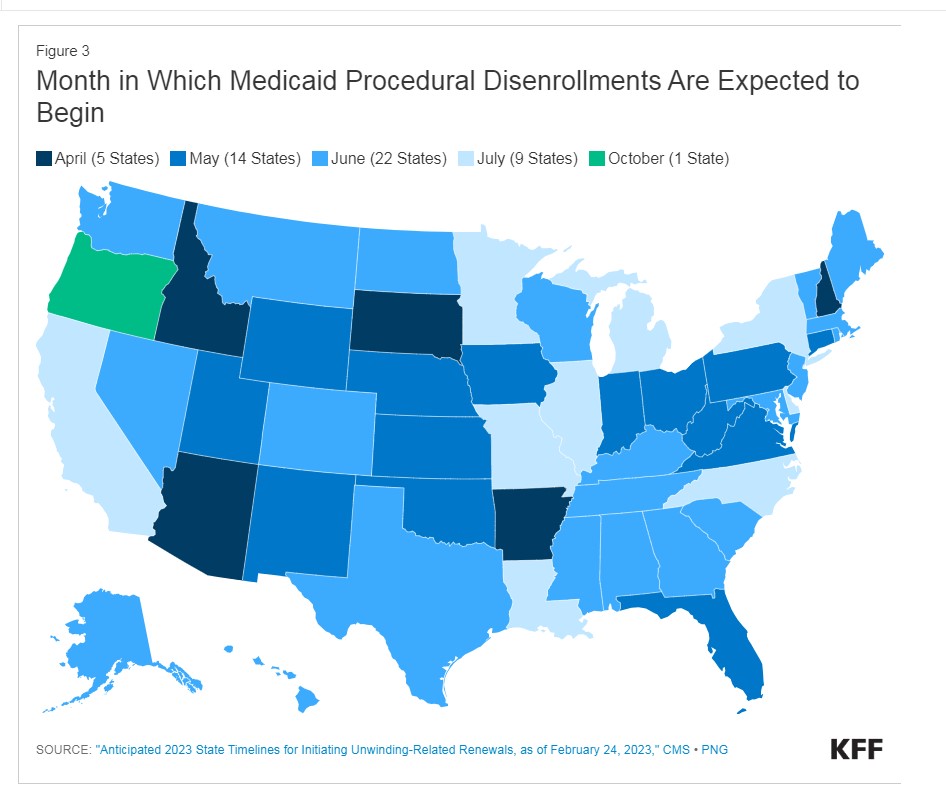
States will begin disenrolling people from Medicaid in different months, with some states resuming disenrollments in April, others in May or June, and even July or later for some states. The figure below shows the month in which disenrollments are expected to begin in each state.




Greg Lindberg loses appeal and could lose much more
How life insurance companies can leverage chatbots
Advisor News
- Americans increasingly worried about new tariffs, worsening inflation
- As tariffs roil market, separate ‘signal from the noise’
- Investors worried about outliving assets
- Essential insights a financial advisor needs to grow their practice
- Goldman Sachs survey identifies top threats to insurer investments
More Advisor NewsAnnuity News
- AM Best Comments on the Credit Ratings of Talcott Financial Group Ltd.’s Subsidiaries Following Announced Reinsurance Transaction With Japan Post Insurance Co., Ltd.
- Globe Life Inc. (NYSE: GL) is a Stock Spotlight on 4/1
- Sammons Financial Group “Goes Digital” in Annuity Transfers
- Somerset Reinsurance Announces the Appointment of Danish Iqbal as CEO
- Majesco Announces Participation in LIMRA 2025: Showcasing Cutting-Edge Innovations in Insurance Technology
More Annuity NewsHealth/Employee Benefits News
- Proxy Statement (Form DEF 14A)
- Idaho Senate approves Medicaid budget
- John Oliver sued by health care boss
- Pharmacy bill passes House committee
- Lowering the cost of insurance in Colorado – a new analysis of the Peak Health Alliance
More Health/Employee Benefits NewsLife Insurance News
- Revised Proxy Soliciting Materials (Form DEFR14A)
- Proxy Statement (Form DEF 14A)
- Exemption Application under Investment Company Act (Form 40-APP/A)
- AM Best Affirms Credit Ratings of CMB Wing Lung Insurance Company Limited
- Council agrees to settlement for animal welfare division
More Life Insurance News